Repeated Oral Ketamine for Depression Treatment – Can Oral Ketamine be used to treat depression?
If you are looking for more information on whether ketamine may help you with your condition, contact us through the web form below or call 703-844-0184
Ketamine is a rapid-acting antidepressant that is FDA approved as Spravato for depression and suicidality. It was developed in 1962 and FDA approved for anesthesia in 1970 as a human drug first and foremost. IV Ketamine has been found to be effective in rapidly reducing depression and suicidality. It is generally given in a dose of 0.5 mg/kg IV over 40 minutes and produces remission or rapid depression reduction within several hours to days in 70% of treatment resistant patients (ones who have failed several medications, ECT, or even TMS).
Why Use several ketamine infusions?
It improves response and lengthens time to relapse of depression:
Shiroma PR, Johns B, Kuskowski M, Wels J, Thuras P, Albott CS, Lim KO. Augmentation of response and remission to serial intravenous subanesthetic ketamine in treatment resistant depression. J Affect Disord. 2014 Feb;155:123-9. doi: 10.1016/j.jad.2013.10.036. Epub 2013 Oct 29. PMID: 24268616.
Study Parameters:
- 14 patients on 2 months of antidepressants
- 6 infusions of 0.5 mg/kg over 40 minutes Monday/Wednesday/Friday schedule
- Monitored for four weeks after for relapse
Results After 6 infusions:
- 91.6% achieved response
- 66.6% had remission of their depression
- 3/14 of patients responded after the first infusion
- After 6 infusions, 4 responded and 6 had remission of depression
- 60% remained as responders 4 weeks after the series of infusions
At NOVA Health Recovery Ketamine Infusion Center, we utilize home based ketamine treatments after the initial series of infusions to maintain response and prevent relapse. Recall that ketamine infusions are frequently used in difficult-to-treat cases that have had long mental health journeys, and ketamine represents a viable option of improvement in mood and functionality whereas other options have failed. Recall the STAR*D Trial that demonstrated poor outcomes for each failed step of therapy in depression:
Rush AJ, Trivedi MH, Wisniewski SR, Nierenberg AA, Stewart JW, Warden D, Niederehe G, Thase ME, Lavori PW, Lebowitz BD, McGrath PJ, Rosenbaum JF, Sackeim HA, Kupfer DJ, Luther J, Fava M. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report. Am J Psychiatry. 2006 Nov;163(11):1905-17. doi: 10.1176/ajp.2006.163.11.1905. PMID: 17074942.
Study Parameters of STAR*D:
- 3671 patients trying four steps of therapy if needed for depression
- If no remission or response with one step of therapy, they would move on to the next step.
- A score of <or=5 on the Quick Inventory of Depressive Symptomatology-Self-Report (QIDS-SR(16)) (equivalent to <or=7 on the 17-item Hamilton Rating Scale for Depression [HRSD(17)]) defined remission; a QIDS-SR(16) total score of >or=11 (HRSD(17)>or=14) defined relapse.
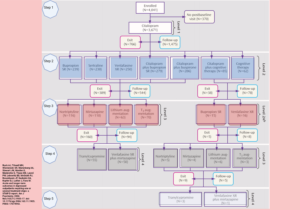
Created with BioRender.com
Results:
- The QIDS-SR(16) remission rates were 36.8%, 30.6%, 13.7%, and 13.0% for the first, second, third, and fourth acute treatment steps, respectively.
- Cumulative Remission Rate: 67%
- Those requiring more treatment steps had higher relapse rates
- Those who responded with remission in the first three steps had lower relapse rates.
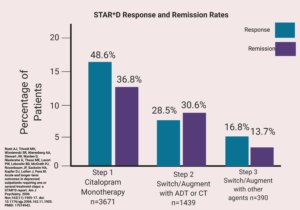
Created with BioRender.com
IV Ketamine Therapy is Highly effective for the treatment of resistant depression based on several meta-analysis:
Ketamine and Other NMDA Antagonists: Early Clinical Trials and Possible Mechanisms in Depression
Newport DJ, Carpenter LL, McDonald WM, Potash JB, Tohen M, Nemeroff CB; APA Council of Research Task Force on Novel Biomarkers and Treatments. Ketamine and Other NMDA Antagonists: Early Clinical Trials and Possible Mechanisms in Depression. Am J Psychiatry. 2015 Oct;172(10):950-66. doi: 10.1176/appi.ajp.2015.15040465. PMID: 26423481.
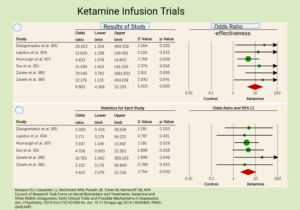
“Ketamine (seven trials encompassing 147 ketamine-treated participants) produced a rapid, yet transient, antidepressant effect, with odds ratios for response and transient remission of symptoms at 24 hours equaling 9.87 (4.37-22.29) and 14.47 (2.67-78.49), respectively, accompanied by brief psychotomimetic and dissociative effects. Ketamine augmentation of ECT (five trials encompassing 89 ketamine-treated participants) significantly reduced depressive symptoms following an initial treatment (Hedges’ g=0.933) but not at the conclusion of the ECT course.”
A recent meta-analysis also demonstrated efficacy of ketamine in depression:
Marcantoni WS, Akoumba BS, Wassef M, Mayrand J, Lai H, Richard-Devantoy S, Beauchamp S. A systematic review and meta-analysis of the efficacy of intravenous ketamine infusion for treatment resistant depression: January 2009 – January 2019. J Affect Disord. 2020 Dec 1;277:831-841. doi: 10.1016/j.jad.2020.09.007. Epub 2020 Sep 7. PMID: 33065824.
This meta-analysis included twenty-eight studies in 35 publications. “A strong ketamine effect was observed within 4 hours following a single infusion, and peaked at 24 hours. Ketamine’s effectiveness was still present, yet somewhat diminished, 7 days post-infusion. Multiple infusions resulted in an enhanced and prolonged ketamine effect.”
Conley AA, Norwood AEQ, Hatvany TC, Griffith JD, Barber KE. Efficacy of ketamine for major depressive episodes at 2, 4, and 6-weeks post-treatment: A meta-analysis. Psychopharmacology (Berl). 2021 Jul;238(7):1737-1752. doi: 10.1007/s00213-021-05825-8. Epub 2021 Mar 31. PMID: 33787963.
This meta-analysis evaluated ketamine therapy for Major Depressive Disorder (MDD) at 2,4 and 6 weeks post-infusion. The meta-analysis observed large effects at 2 weeks (g = −1.28), 4 weeks, (g = −1.28), and 6 weeks (g = −1.36) post-treatment. This analysis showed that ketamine can be an effective pharmacologic intervention for major depressive episodes, with treatment effects lasting up to 6 weeks post-ketamine administration, which has many positive implications for treatment,
The Real question is how to prolong the effectiveness of ketamine?
Thus far, the best option is with booster infusions. Generally, between every 2-4 weeks, a repeat ketamine infusion may be effective in maintenance of remission for MDD. A recent study below addressed the utility of repeated ketamine infusions for relapse prevention in MDD:
Strategies to Prolong Ketamine’s Efficacy in Adults with Treatment-Resistant Depression
McMullen EP, Lee Y, Lipsitz O, Lui LMW, Vinberg M, Ho R, Rodrigues NB, Rosenblat JD, Cao B, Gill H, Teopiz KM, Cha DS, McIntyre RS. Strategies to Prolong Ketamine’s Efficacy in Adults with Treatment-Resistant Depression. Adv Ther. 2021 Jun;38(6):2795-2820. doi: 10.1007/s12325-021-01732-8. Epub 2021 Apr 30. PMID: 33929660; PMCID: PMC8189962.
In this study, twenty-two articles were included: ten randomized controlled trials (RCTs), eight prospective open-label trials, one retrospective chart review, and three case reports. “Different treatment modalities including pharmacological interventions, manualized-based psychotherapies, electroconvulsive therapy, transcranial magnetic stimulation, and intravenous monotherapy were examined to determine their impact on the prolongation of antidepressant effects following acute ketamine treatment. No treatment modality, other than repeat-dose IV ketamine, has demonstrated ability to significantly prolong the acute efficacy of IV ketamine in Treatment Resistant Depression.”
Other considerations to maintain efficacy of ketamine infusions is to utilize ketamine as home-based intranasal and oral ketamine troches. One study below demonstrates repeated oral ketamine can be effective in out-patient treatment resistant depression:
Domany, Y., Bleich-Cohen, M., Tarrasch, R., Meidan, R., Litvak-Lazar, O., Stoppleman, N., . . . Sharon, H. (2019). Repeated oral ketamine for out-patient treatment of resistant depression: Randomised, double-blind, placebo-controlled, proof-of-concept study. British Journal of Psychiatry, 214(1), 20-26. doi:10.1192/bjp.2018.196
- Randomized Controlled Study of 22 patients for treatment and 19 for control
- Ketamine treated patients had a decrease in depression at all time points.
- 27 % of ketamine oral treated patients achieved remission versus none of the controls
- Number needed to treat is 3.7 (awesome)
- Few side effects
- Conclusions: Repeated oral ketamine produced rapid and persistent amelioration of depressive symptoms in out-patients with TRD and was well tolerated. These results suggest that add-on oral ketamine may hold significant promise in the care of patients suffering from TRD in the community.
More Recently, Nature Magazine featured an open-label trial demonstrating efficacy of oral ketamine for chronic suicidality:
Low dose oral ketamine treatment in chronic suicidality: An open-label pilot study
This study included 32 adults (aged 22–72 years; 53% female) with chronic suicidal thoughts that participated in the Oral Ketamine Trial on Suicidality (OKTOS), an open-label trial of sub-anaesthetic doses of oral ketamine over 6 weeks. Participants began with 0.5 mg/kg of ketamine, which was titrated to a maximum 3.0 mg/kg. Follow-up assessments occurred at 4 weeks after the final dose. They utilized the Beck Suicidal ideation scale as a primary measure.
- Clinical improvement was 69% in the first 6 weeks
- 50% had significant improvement at week 10
- Conclusion: Six weeks of oral ketamine treatment in patients with chronic suicidality led to significant reduction in suicidal ideation.
Impact of oral ketamine augmentation on hospital admissions in treatment-resistant depression and PTSD: a retrospective study Hartberg J, Garrett-Walcott S, De Gioannis A. Impact of oral ketamine augmentation on hospital admissions in treatment-resistant depression and PTSD: a retrospective study. Psychopharmacology (Berl). 2018 Feb;235(2):393-398. doi: 10.1007/s00213-017-4786-3. Epub 2017 Nov 18. PMID: 29151192.
- This was a retrospective review of 37 patients receiving oral ketamine and demonstrated that inpatient hospital days were reduced by 70% and hospital admissions were reduced by 65%.
- This trial utilized 14 subjects receiving ketamine 0.5 mg/kg orally over 28 days and rated with the Hospital Anxiety and Depression Scale at days 3,7,14,21, and 28.
- Results showed improvement in depression and anxiety for 8 patients in the trial and 100 % of the patients had response.
- Improvements lasted throughout the 28 days.
- Side effects: Diarrhea, trouble sitting still, and insomnia
Oral Ketamine for Depression, 1: Pharmacologic Considerations and Clinical Evidence
The above article is a review of oral ketamine as well.
Finally, ketamine infusions can be used at the beginning of depression therapy to make initial antidepressant therapy more rapidly effective.
- 30 patients with MDD (HAMS-D scale>24)
- 4 weeks randomized double-blind treatment excitalopram (10 mg/day) and IV Ketamine (0,5 mg/kg over 40 minutes) or escitalopram 10 mg/day + placebo infusion.
- Depressive symptoms were measured using the Montgomery–Asberg Depression Rating Scale (MADRS) and the Quick Inventory of Depressive Symptomatology – Self-Report (QIDS-SR). Suicidal ideation was evaluated with the QIDS-SR item 12.
- Adverse psychopathological effects were measured with the Brief Psychiatric Rating Scale (BPRS)-positive symptoms, Young Mania Rating Scale (YMRS) and Clinician Administered Dissociative States Scale (CADSS).
Conclusion of Trial: By 4 weeks, more escitalopram + ketamine-treated than escitalopram + placebo-treated patients responded (92.3% v. 57.1%, p = 0.04) and remitted (76.9% v. 14.3%, p = 0.001), with significantly shorter time to response [hazard ratio (HR) 0.04, 95% confidence interval (CI) 0.01–0.22, p < 0.001] and remission (HR 0.11, 95% CI 0.02–0.63, p = 0.01).
At 4 weeks:
- 92% of ketamine+ escitalopram patients responded versus 57% escitalopram patients
- 76.9% of ketamine+ escitalopram patients remitted versus 14% of escitalopram patients.
- Remission and response occurred at a more rapid rate with ketamine treatment.
- Single-dose i.v. ketamine augmentation of escitalopram was safe and effective in severe MDD, holding promise for speeding up early oral antidepressant efficacy.
Conclusions:
- Ketamine is rapidly effective in a significant number of patients with treatment resistant depression
- A series of infusions works best for depression response
- Booster infusions work for maintenance of antidepressant effect
- Oral ketamine (and home-based intranasal ketamine) can be used as a maintenance strategy as well.
- Ketamine IV can be used in early depression treatment to make antidepressant use more rapidly effective and increase remission rates.
.
: